Revision Total Hip Arthroplasty
Español - TBDIntroduction to revision surgery
Hip replacement surgery is effective for relieving the pain and disability of osteoarthritis of the hip. Over 300,000 primary (first time) total hip replacements are performed in the United States each year.
As many “baby boomers” reach retirement age and live longer, it is expected that nearly 600,000 hip replacements will be performed annually by 2030.
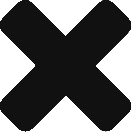
While most hip replacements last for many years some patients need to have a second operation or “revision” surgery during the course of their lifetime (Figure 1). Revision surgery can be a more complex procedure where some or all of the components may need to be removed and replaced. Revision surgery may take longer than a primary total hip replacement and require the use of special tools and implants.
Printer Friendly
Why would I need revision hip surgery?
In 2018, an estimated 9,000 total hip revision surgeries were performed in the United States. Most were done for the following reasons:
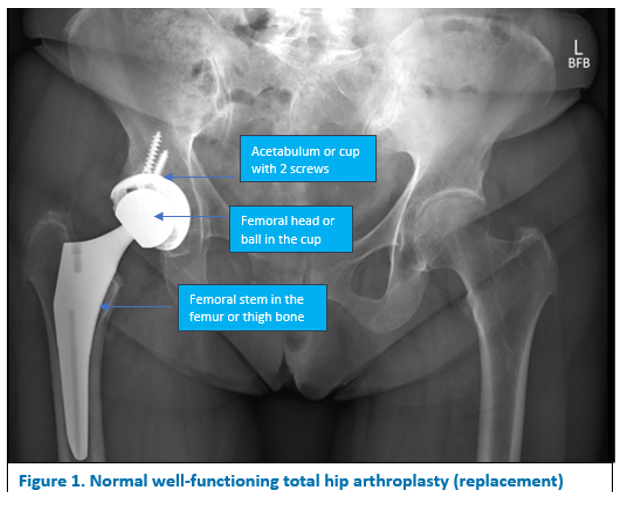
- – Loosening– The components wear, break, or become loose from their attachments to the surrounding bone (Figure 2).
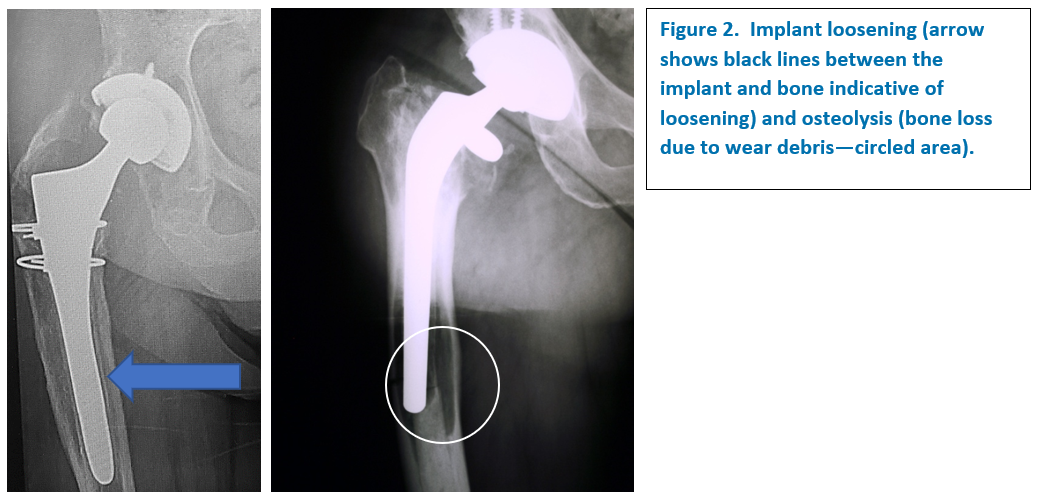
- – Dislocation –Dislocation is a problem where the ball of the hip joint comes out of the socket or “dislocates” (Figure 3). Most often your surgeon can manipulate the hip back in place under anesthesia.
Revision may be necessary if the ball does not go back, and your surgeon has to reopen your hip. He or she may change the position of one or more components to make the hip more stable. Revision may also be done in cases where there have been multiple dislocations over a period of time.
- – Infection – Infection of a total hip replacement may develop right after surgery or even years later if the infection comes from another part of the body. An early or superficial infection may sometimes be treated by draining the wound (“washing” it out) and taking antibiotics through an IV or by mouth for a period of time afterwards. If the infection is deep and/or has been going on for a long time, the components may need to be removed to treat the infection. A temporary implant called a spacer, coated with antibiotic cement, is typically inserted for several months until the infection has been treated. A new permanent implant can then be placed when the temporary spacer is removed if it appears the infection has been treated. This process is commonly referred to as a 2-stage exchange procedure with the first stage being the removal of the infected implants with spacer placement and the second stage being implantation of long-term implants with spacer removal once the infection has been treated.
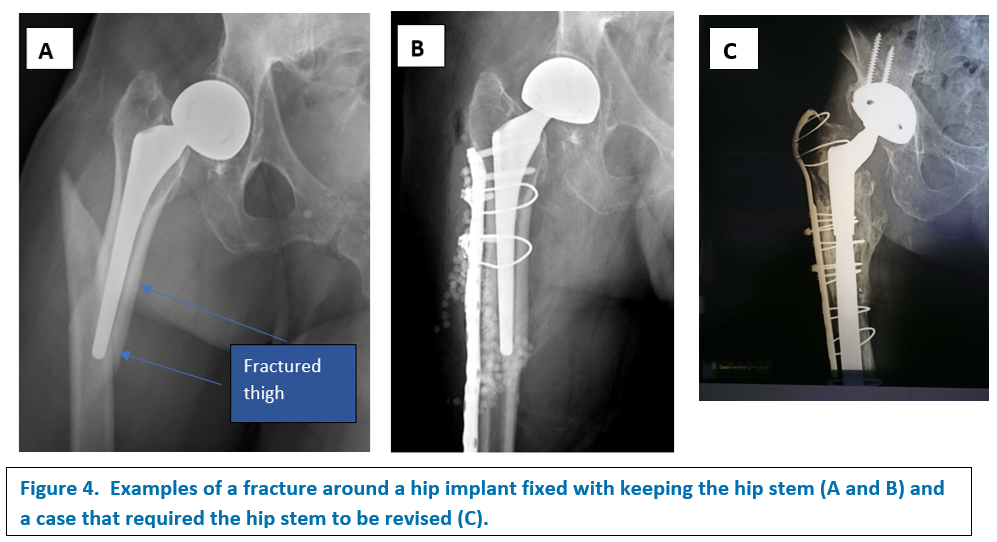
4 – Fracture – A total hip replacement may be functioning well, but a fall or other injury can fracture the hip or upper part of the femur. The hip replacement parts may remain well-fixed in the bone, or the fracture can cause the implants to become loose. If the bone remains well healed to the femoral stem (bottom part of a total hip replacement), the surgeon can typically keep the hip replacement parts and fix the broken bone with plate and screws (Figure 4a and 4b). If the implants are failing and/or are loose, some of the components may need to be replaced to repair the fracture and make the bone more stable (Figure 4c).
To summarize the causes for revision surgery, according to the 2020 AAOS American Joint Replacement Registry, the four main reasons for hip revision surgery are (percent of all revisions performed in the registry):
- Infection 19.3%
- Dislocation 17.4%
- Implant Loosening 15.8%
- Fracture 8.9%
What does revision hip surgery entail—How is it different from my first surgery?
A revision hip replacement is typically more technically difficult than the initial replacement surgery. A longer incision is generally required. Scar tissue can make it harder to expose (see) the joint and the implants. Structures such as nerves and vessels may be buried/hidden in scar and have to be carefully identified during the procedure.
Wider surgical exposure (dissection) is required. All (full revision) or some (partial revision) of the components must be removed or exchanged. If a component is well fixed to bone but needs to be removed, it must first be separated from the bone. If the component was originally cemented into place, extensive work may be required to remove all of the cement down to fresh healthy bone.
In many cases, the only way to remove a well–fixed femoral component from the femur is to make a long cut in the bone called an osteotomy. An osteotomy is a planned and controlled fracture where the bone is opened like a book and the implant removed. The goal of an osteotomy is to control the process for implant removal and avoid more damage by accidentally causing a fracture. This part of the procedure is performed carefully to make sure the bone will support the new implants. The fractured bone is then repaired at the end of surgery (the book is then closed). Over time, the goal is for the bone pieces to heal to the implant and to each other to provide stability to the new implant.
Often in revision cases there has been bone loss. This can be due to infection or digestion of the bone by irritated white blood cells through a process called osteolysis. This means bigger and longer implants are needed to get adequate fixation in the remaining bone. When there is not enough bone to support the new components, bone grafting may be necessary. The bone can either come from your own body (autograft) or from a bone bank (allograft or bone from a cadaver source). In some cases, extra plates, screws, or wires are needed to hold a bone graft in place.
Since the incision is longer, the exposure wider, and the components larger, a revision procedure will usually take longer than primary surgery.
What will my recovery look like?
The time for recovery from a revision procedure depends on your strength and physical condition as well as the extent of the surgical procedure.
Often the recovery from a revision procedure is similar to the primary surgery. You get out of bed on the day of surgery or the day after surgery and start physical therapy. You may begin bearing weight with a walker or crutches and
advance to a cane as you are comfortable. In some cases, your weightbearing may be limited so that only part of your weight can be placed on your revised joint. Even though it may take 2 to 4 months to fully recover, you may be moving about and performing your normal activities within a few days or weeks.
In more difficult cases, however, the recovery will be longer. This is because the incision is longer, and more muscle and soft tissues are divided to gain exposure. As a result, the muscles may be weaker after surgery and require a longer rehabilitation. Recovery also depends on what condition you are in prior to surgery to include your fitness level, strength and ability to walk. A patient who has been wheelchair bound for six months will likely have a longer recovery than a patient who was walking independently prior to the surgery.
If bone grafting is required or your surgeon has to do an osteotomy, you may need to limit weight-bearing for several weeks or even months until the bone has healed is strong enough to hold your body weight. This may also be true if time is required for the components to bond to the bone until they are stable.
As a rule, revision surgeries are more complex and may be more painful so recovery may take longer.
What are the possible complications?
Like primary surgeries, most revision procedures do well and last a long time with no complications. But since revisions are more complex the complication rates are higher. The most common complications include:
Infection – In primary hip replacements the risk of infection is less than 1%. The risks of infection are greater with bigger procedures and in hips that have had multiple operations. Infection after a revision surgery can range between 3 and 5%. Additionally, revision surgery for infection has a higher rate of failure than revision for other causes.
Dislocation – Since hip revisions are more extensive procedures with larger components and there is greater muscle damage, the risk of dislocation is higher. Whereas hip dislocations may occur in fewer than 2% of primary surgeries the risk of dislocation in revisions may be close to 10%.
Ectopic bone or Heterotopic Ossification– Hips that have had multiple surgeries may grow extra bone around the joint. This is called ectopic bone (Heterotopic = other place and Ossification = bone formation) or bone growing in the wrong place. If there is a large amount of extra bone it may be painful and limit motion of the joint.
Nerve or vascular injury – Some of the nerve and vascular structures that are easily visible or protected during primary surgery may be covered in scar tissue during a revision. This means they are more susceptible to injury. The sciatic nerve in particular may be stretched or injured. If this happens, there may be some loss of function in the leg and foot which can be either temporary or permanent.
Revision Wrap-up
Most joint replacements will last for many years. However, as more younger patients choose to have surgery, the need for revision procedures in the future may be greater. Since revisions are longer and often more complicated, the long-term results may not be as good as the results from primary surgery.
Do not hesitate to ask questions. Your surgeon can explain the risks, benefits, and recovery time for a revision procedure.
This article has been written by Stuart J. Fischer, MD, in collaboration with the AAHKS Patient and Public Relations Committee and peer reviewed by the AAHKS Evidence Based Medicine Committee. Links to these pages or content used from the articles must be given proper citation to the American Association of Hip and Knee Surgeons.